Vasectomy overview
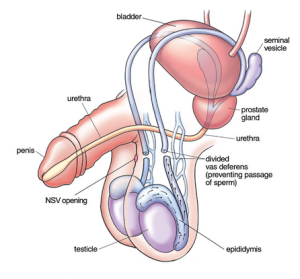 A vasectomy (male sterilisation) is a minor surgery to cut or seal the tubes that carry a man’s sperm to permanently prevent pregnancy. Men will continue to ejaculate, but sperm is no longer in the semen.
A vasectomy (male sterilisation) is a minor surgery to cut or seal the tubes that carry a man’s sperm to permanently prevent pregnancy. Men will continue to ejaculate, but sperm is no longer in the semen.
Before getting a vasectomy you need to be certain you don’t want to father a child in the future. Although vasectomy reversals are possible, vasectomy should be considered a permanent form of male contraception.
Vasectomy offers no protection from sexually transmitted infections.
Guidelines recommend to carry out vasectomy under local anaesthetic, where you’re awake but don’t feel any pain, and takes about 15 minutes.
Vasectomy guidance does not recommend for this procedure to be carried out under general anaesthetic, but the option exists for very anxious patients or surgically challenging cases.
Vasectomy is considered a very safe minor surgical procedure with overall low side effect and high satisfaction rates by men (1).
Summary: Advantages and disadvantages of a vasectomy
Advantages:
- a vasectomy is more than 99% effective at preventing pregnancy
- It is inexpensive when compared with most other contraception and many countries fund free vasectomies.
- long-term effects on your health are rare
- it doesn’t affect your hormone levels, sex drive or interfere with the enjoyment of sex
- You’ll still have erections and ejaculate, but your semen won’t contain sperm.
- it may be chosen as a simpler and safer alternative to female sterilisation
- It’s considered permanent, so once it’s done you don’t have to think about contraception again.
- It is an extremely sustainable form of contraception (no water pollution with hormones, no reviews, no replacement of contraception required)
Disadvantages:
- You’ll need to use contraception for at least 12 to 20 weeks after the operation, because sperm will still be in the tubes leading to the penis.
- A vasectomy can’t be easily reversed, and reversals are rarely funded by the NHS
- you need to keep using contraception after the operation until tests show your semen is free of sperm
- possible complications include a collection of blood inside the scrotum (haematoma), hard lumps called sperm granulomas (caused by sperm leaking from the tubes), an infection, or long-term testicle pain (you may need further surgery)
- the vas deferens tubes can reconnect, but this is very rare
- vasectomy doesn’t protect against STIs, so you may need to use condoms as well
- Your ball sack (scrotum) can occasionally become bruised, swollen or painful – Rarely, in about 1 in 500 cases some men have ongoing pain in their testicles.
Get the process started or read on…
How a vasectomy is carried out
A vasectomy is a quick and relatively painless surgical procedure. In most cases, you’ll be able to return home the same day.
There are 2 types of vasectomy:
- a conventional vasectomy using a scalpel (surgical knife)
- a so called “no-scalpel vasectomy (NSV)“. A more modern, but less well known name is also “Minimally Invasive Vasectomy (MIV)”
The doctor doing your vasectomy will discuss which option he or she can provide for you. However, guidelines suggest NSV or MIV to be the preferred procedure due to its lower side effect rates (2).
Vasectomy and No-Scalpel Vasectomy in Detail
Differences between No-Scalpel (minimally invasive) and conventional vasectomy
Conventional vasectomy
The doctor first numbs your scrotum with a local anaesthetic. They then make 2 cuts in the skin on each side of your scrotum to reach the tubes that carry sperm out of your testicles (vas deferens).
Each tube is cut and a small section removed. The ends of the tubes are then closed, usually by tying them.
The cuts are stitched, usually using dissolvable stitches or clips that go away on their own within about three to six weeks.
No-scalpel vasectomy (NSV) = minimally invasive vasectomy (MIV)
The doctor first numbs your scrotum with local anaesthetic. They then make a tiny puncture hole in the skin of your scrotum to reach the tubes. This means they don’t need to cut the skin with a scalpel.
The tubes are then gently cauterised and some surgeon prefer an “open ended method”, at least to the lower vas. The upper vas end is often sealed with heat or radiofrequency cautery or a stitch or clip to avoid sperm entry. A piece of vas may be removed.
There’s little bleeding and in the classic No-Scalpel Vasectomy there are no stitches with this procedure. It’s thought to be less painful and less likely to cause complications than a conventional vasectomy.
Before your vasectomy procedure
A modern service should give you a modern and good information before your vasectomy. Good services also tend to aid their vasectomy decision making with videos, webinars, online resources. They should give you very thorough information well in time before your vasectomy, so you can sit back and reflect. Depending on how modern your chosen service is this may be done via a face to face consultation, telephone consultation or online consultation. You should be given a good amount of information in writing so you can read the information, reflect and make your own decision.
Your doctor will ask you to consider a lot of issues, provide information, and ensure you are giving informed consent. There are plenty of reasons not to have a vasectomy (click here for more information) and there are also plenty of other contraceptive choices (click here for a summary)
You should only have a vasectomy if you’re certain you don’t want any more children or don’t want children at all. Interstingly, a new study shows men without children are less, not more likely, to regret a vasectomy decision and are generally very happy with their decision. (Click here for this new study). However, generally, men und 30 are more likely to regret a vasectomy decision. Generally 7% of men regret their decision of a vasectomy. this rises to 11% in men under 30 years of age (Click here for evidence).
If you have a partner, discuss it with them before you decide. If possible, you should both agree to the procedure, but it’s not a legal requirement to get your partner’s permission.
GPs / family practitioners can refuse to refer you for a tax payer funded vasectomy on the NHS if they think it is not in your best interest. However, neither age nor the lack of a partner or the lack of children should really be a barrier to vasectomy.
During the procedure
- Vasectomy surgery usually takes about 10 to 30 minutes although your time at the clinic is usually 30-60 minutes including the aftercare and some time to rest. To perform a vasectomy, your doctor will likely follow these steps:
- Invite you into the treatment room and talk to you about any remaining concern you have. Doctor and staff should introduce themselves.
- Clean their hands, put on masks (some services may offer your a mask for infection prevention) and cleanse you with a mild disinfectant.
- They will drape the area and secure the penis away from the surgical area to minimise the risk of injury.
- They will numb the surgery area by injecting a local anaesthetic into the skin of your scrotum with a small needle.
- Secure your first vas deferens
- Create a small opening in the upper part of your scrotum once the surgery area is numb. With the “no-scalpel” technique (NSV), there is typically a small puncture (using a metal haemostat or electrosurgical equipment) instead of an incision.
- Withdraw part of the vas deferens through the incision or puncture.
- Interrupt and / or cauterise the vas. Some surgeons remove a part, some don’t, some cauterise internally, some externally. Some use a clip or a suture, some do not use any foreign bodies. There are as many techniques as there are surgeons.
- The same process is repeated on the other side although in NSV only one incision / opening / puncture is used.
- Close the incision at the surgery area. Stitches or glue may be used in conventional vasectomy. In No-Scalpel vasectomy the wound is usually so small it is typically left to close on its own over time. Some services apply a silicone plaster to aid healing.
After your vasectomy procedure – Recovering after the operation
Painkillers
It’s common to have some mild discomfort, swelling and bruising of your scrotum for a few days after the vasectomy. You can take painkillers, such as Paracetamol (Acetaminophen in the US), to help. See a GP if it’s still painful after taking painkillers.
Underwear
Wear snug fitting underwear day and night for the first few days to help support your scrotum and ease any discomfort or swelling. Make sure you change your underwear every day.
Hygiene
Usually it is wise not to bring water onto your wound for 48 hrs. After that it is safe to shower, but bath and pool water can be contaminated and it is probably wise not to bathe for a week or so. Click here for more information about postoperative hygiene
Returning to work
You can usually return to work 1 or 2 days after a vasectomy, but should avoid manual labour, sport and heavy lifting for at least a week after the procedure to prevent complications. See a GP if you still have symptoms after a few days.
Having sex
Treat sex like any other exercise and avoid sexual activity for at least 7 days after having a vasectomy. You’ll need to use another method of contraception for at least the first 8 to 12 weeks, as it can take this long to clear the remaining sperm in your tubes. How long this takes varies from man to man. There’s still a risk of pregnancy during this time. It’s common to have blood in your semen in the first few ejaculations after a vasectomy. This isn’t harmful.
How will I know if my vasectomy has worked – Testing after vasectomy
Delayed protection
Patience is a virtue – also in semen sampling
The time for sampling has come
Stopping additional contraception
Some men may need more than 1 test and some surgeons request 2 tests from their patients. Until it’s been confirmed that your semen is free of sperm, continue to use another form of contraception.
A little dead sperm does not make a big difference
A few men will continue to have small numbers of sperm in their system, but these sperm don’t move and are less likely to make your partner pregnant. Doctors tend to ignore low numbers of dead (immotile) sperm. If you’re one of these men, your doctor will tailor their advice depending on a number of factors including number of dead sperm and other factors.
Vasectomy Failure
The test also helps to identify the rare cases in which the tubes naturally rejoin themselves. This chance is probably approximately 1:200 to 1:800 and in average 1:500.
Late Vasectomy Failure
The risk of late failure (failure to father a child following clearance) is claimed to be approximately 1:2000 and a large UK based audit study recently confirmed this figure (1). This figure appears to be higher if clearance is given too early after vasectomy and late healing sets in after a patient has their letter of clearance. It appears lower when a semen sample is done later and a service waits longer to confirm a patients sterile.
How much should I pay for a vasectomy
You can get good vasectomy surgeons of your choice for the following fees:
- USA: Approximately $700
- Europe: Approximately € 600
- UK: Approximately £500
How long will I have to wait for vasectomy operation?
- Private services should be able to offer you an appointment within 1-4 weeks. Otherwise they may not be well led and efficiently run.
- In some parts of the UK, a vasectomy is available free of charge through the NHS. But waiting lists can be up to 2 years, depending on where you live.
- Speak to your GP or ask at your local contraception clinic for more information on NHS vasectomies. As waiting lists for vasectomies can be long, some men choose to pay to have the procedure carried out privately.
- You can request a doctor or surgeon of a specific sex, but this may mean having to wait longer.
Risks of vasectomy
Change of mind
A potential concern with vasectomy is that you might later change your mind about wanting to father a child.
Although it might be possible to reverse your vasectomy, there’s no guarantee it will work. Reversal surgery is more complicated than vasectomy, can be expensive and is ineffective in some cases. Reversal is generally 10 times more expensive than vasectomy, yet it appears probably still the cheapest option.
Freezing sperm is possible, but you can only freeze so much sperm and not always will frozen sperm easily lead to a pregnancy even when inserted at the optimum time. Then IVF may be come necessary.
Other techniques also are available to father a child following vasectomy, such as in vitro fertilisation (IVF / ICSI). However, these techniques are expensive and not always effective.
Sperm retrieval is possible and the methods are multiple, but finding a specialist for a particular method may be difficult.
More common early side effects after vasectomy (but still only 1% in good surgeons) can include:
- Bleeding or a blood clot (hematoma) inside the scrotum
- Blood in your semen
- Bruising of your scrotum
- Infection of the surgery site
- Usually mild to moderate pain or discomfort
- Swelling
- Pain as a side effect can be minimised through the so called No-Scalpel Vasectomy (NSV) also called Minimally invasive vasectomy (MIV)
Delayed complications may include:
Unfounded concerns about vasectomy
Many men worry that a vasectomy could cause serious problems — but these fears are unfounded. For example, a vasectomy won’t:
- Affect your sexual performance. A vasectomy won’t affect your sex drive or your masculinity in any way. You will still produce the same amount of testosterone, because the surgeon only interrupts the tubes carrying the sperm and leaves the testicle, which produces testosterone, alone. Men have even reported higher sexual satisfaction after a vasectomy, because the worry about getting somebody pregnant is gone.
- Permanently damage your sexual organs. There’s very little risk that your testicles, penis or other parts of your reproductive system will be injured during surgery. In extremely rare cases, injury to the blood supply can lead to the loss of a testicle. This is a very rare event for a skilled vasectomy surgeon.
- Increase your risk of certain cancers. Although there have been some concerns about a possible link between vasectomy and testicular or prostate cancer in the past, there’s no proof vasectomy causes prostate or testicular cancer and causality has never been shown. Click here for more information
- Increase your risk of heart disease. As with cancer fears, there doesn’t appear to be any link between vasectomy and heart problems.
- Cause severe pain. Occasionally you might feel minor pain and pulling or tugging during surgery, but severe pain is rare. Likewise, after surgery you might have some pain, but for most men the pain is minor and goes away after a few days.
References
(2) A comparative study of the no scalpel and standard incision approaches to vasectomy in 5 countries. The Male Sterilization Investigator Team
